
Objectives
This study examines the first six months of the CirrusMD telemental health clinic — from June through December 2020 — to determine its effects in treating mental health, as measured by patients with Generalized Anxiety Disorders using GAD-7, as well as patients with depression, using PHQ-9.
The study also analyzes the impact of telemental healthcare provided by primary care clinicians using a care plan modeled by licensed psychiatrists.
Overview of the CirrusMD Telemental Health Program
As the demand for mental healthcare services continues to increase in the U.S., access to qualified healthcare professionals has not been able to match demand. To help bridge gaps in mental healthcare access, CirrusMD began formally delivering telebehavioral health care in June 2020 during the COVID-19 pandemic.
Services are delivered via a secure, HIPAA-compliant platform, which connects patients with a live physician who is part of an integrated telehealth network of multi-specialty doctors. Consultations that begin through text messaging can transition to audio or video conferencing when necessary.
This study contains the first six months of results for patient encounters on the CirrusMD platform related to depression and anxiety disorders. Analysis of CirrusMD data demonstrates that patients receiving behavioral healthcare and who are actively engaged in teletherapy treatment are improving and realizing clinically meaningful changes in their mental health outcomes. This is reported subjectively and objectively through measurement-based outcomes using PHQ-9 and GAD-7 data.
Background
DEPRESSION:
Primary care physicians are more likely to see patients with depression than with any other health disorder except hypertension. Depression has been ranked as the leading cause of disability and premature death among people aged 18 to 44 and is a leading cause of disability for people of all ages (6,7,8).
Once depression is identified and treated with medication, nearly half of patients receiving an initial prescription for an antidepressant discontinue treatment during the first month, and few receive the recommended levels of follow-up mental health services (8,10,11).
ANXIETY:
Generalized Anxiety Disorder (GAD) is a chronic, debilitating mental illness associated with marked impairment in daily functioning (12,13). Chronic worry is consistently found in 10% of the population, with a level of anxiety and tension so significant that it impairs daily function. The robust association of GAD with psychological and physical comorbidities contributes to the complexity of the illness and its limited treatment success (13,17,18).
More than 90% of patients with GAD present with an additional psychiatric diagnosis; most patients with severe GAD have been ill on average 15 years before seeking help. The majority of patients with GAD present to their primary care physician with a somatic complaint seemingly unrelated to GAD, which creates another potential barrier to treatment (13,17).
Screening Tools
DEPRESSION:
The Patient Health Questionnaire-9 (PHQ-9) satisfies five practical considerations: brief, self-administered, multipurpose, in the public domain and easy to score. Scores of 5, 10, 15 and 20 on the PHQ-9 represent thresholds of mild, moderate, moderately-severe and severe depressive symptoms, respectively (1).
ANXIETY:
The GAD-7 scale has good reliability, as well as criterion, construct, factorial and procedural validity. Increasing scores on the scale are strongly associated with functional mental health impairment. A score of 10 or greater represents a reasonable cut point for identifying cases of GAD. Cut points of 5, 10, and 15 can be interpreted as representing mild, moderate and severe levels of anxiety on the GAD-7.
Telemental Health Services
In the CirrusMD integrated model, physicians identify potential behavioral health concerns through targeted questions. Based on patient responses, they may administer standardized assessment tools — such as the GAD-7 (for anxiety) and PHQ-9 (for depression) — to determine what treatment interventions are needed. During a single telemental health encounter, the healthcare provider can discuss medications with the patient, seek guidance with a CirrusMD psychiatrist, and make a recommendation for follow-up care, all in real time.
After the initial telepsychiatry encounter, CirrusMD Primary Care and Specialty (PCS) team doctors, including family medicine and psychiatry physicians, proactively follow up with the patient to ensure that symptoms are improving. They track GAD-7 and PHQ-9 data, and if needed, adjust medications and provide direction to additional behavioral health services.
Contact is made at 2, 4, 6 and 8 weeks. Frequent contacts during the follow-up period have been associated with better outcomes. Patients should be seen by mental health providers 2 weeks after starting medications to assess medication acceptance and response, adverse effects and suicide risk, as well as to provide patient education and additional health information. After initial identification, three contacts within 12 weeks are considered ideal.
Report data from our study indicated that the CirrusMD PCS team had a mean of 4.41 contacts with patients over an 8.1 week period.
Defining Outcomes
DEPRESSION:
A 5-point change in PHQ-9 score is clinically significant. Full remission is defined as a PHQ-9 of less than 5 (14,15,16). Partial remission is defined as a PHQ-9 of less than 10. Using the PHQ-9 to assess response after 4 to 6 weeks of adequate pharmacotherapy, change is categorized in 3 buckets:
- Decrease of 5 points: adequate or complete response
- Decrease of 2 to 4 points: partial response
- Decrease of 1 point or no change: poor or no response
ANXIETY:
When using the GAD-7 to track changes over time, severity is tracked using the total score; meaningful change is defined as a GAD-7 change of 5 or more points. A score of less than 5 represents remission (2).
Results
PHQ-9 and GAD-7 data was analyzed for the telemental health patients cared for from June-December 2020 in the CirrusMD PCS Clinic. Patients were from commercial health insurance plans, Medicaid/high ED utilizers, and employer groups both insured and uninsured.
DEPRESSION:
PHQ-9 Results (N = 317) | A nonparametric statistical method called the Wilcoxon rank sum analysis was used to analyze the PHQ-9 statistical data. The Wilcoxon Ranked Sum analysis shows that the decrease between initial and final PHQ-9 patient scores is highly significant (p < 0.0001, 95% CI 4.5 to 6.0, Median score decreased 5.5 points). There is a trend for a lower PHQ-9 score correlating to more chats related to the patient’s mental health concerns as well as with the overall duration of the treatment episode, although this finding did not reach statistical significance.
- The overall mean initial PHQ-9 score was 16.723 (moderately-severe range)
- Over a mean of 8.1 weeks and a mean contact of 4.41 times to discuss mental health issues. Patients saw an improvement in PHQ-9 scores by a reduction of 7.71 points. The overall mean final PHQ-9 score was 9.017 (mild range).
- This reduction by 7.71 points represents a clinically significant change and is an adequate or complete response.
Additional findings included:
- Patients with a PHQ-9 reduction of at least 5 points (indicating a complete or adequate response) was 72.204%
- Patients meeting partial response (a PHQ-9 change of 2-4 points) was 14.377%
- Patients with no response (indicated by a change of less than 2 points) was 13.419%
- 22% of patients met criteria for full remission (a final PHQ-9 less than 5)
- 41.853% met criteria for partial remission (a final PHQ-9 score less than 10)
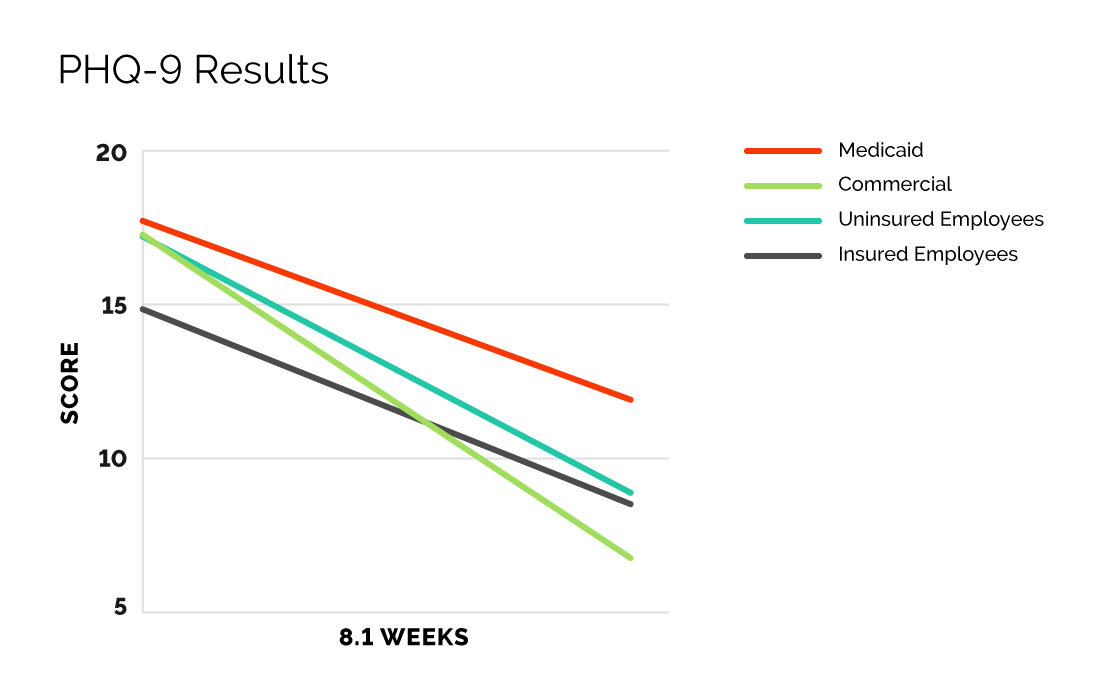
Depression Results by Plan Type
- Patients with commercial health insurance plans averaged initial PHQ-9 scores of 17.27, reducing to 6.77 or a change of 10.5 points
- Employer uninsured patients averaged initial PHQ-9 scores of 17.21, reducing to 8.89 or a change of 8.321 points
- Employer insured patients averaged initial PHQ-9 scores of 14.85, reducing to 8.52 or a change of 6.33 points
- Medicaid/ED High Utilizer patients (defined by 2 or more ED visits in the past 12 months) averaged initial PHQ-9 scores of 17.72, reducing to 11.91 or a change of 5.81 points
ANXIETY:
GAD7 Results (N = 332) | A nonparametric statistical method called the Wilcoxon rank sum analysis was used to analyze the GAD-7 statistical data. The Wilcoxon Ranked Sum analysis shows that this decrease in initial to final GAD-7 scores is highly significant ( p < 0.0001, 95% CI 4.0 to 5.5 Median score decreased 4.5 points). There is a trend for a lower GAD-7 score correlating with more chats related to the patient’s mental health concerns although this did not reach statistical significance. The trend for lower GAD-7 scores with the number of days treated nears statistical significance.
To measure outcomes for anxiety, we used data that measures change in initial and final GAD-7 scores. Initially, the overall mean GAD-7 score was 15.058 (just within the severe range). Over a mean of 8.1 weeks and 4.41 behavioral health encounters, these patients saw a reduction in GAD-7 scores of 6.945 points.
- The overall mean final GAD-7 score was 8.112
- The overall point reduction of 6.945 showed a clinically meaningful reduction
- 68.343% patients saw a GAD-7 point reduction of at least 5 points
- 31.657% of patients did not meet the definition of clinically meaningful response
- 26.923% of people reached full remission during this 8 week period
- 42.9% attained some partial remission, with GAD-7 scores of < 10
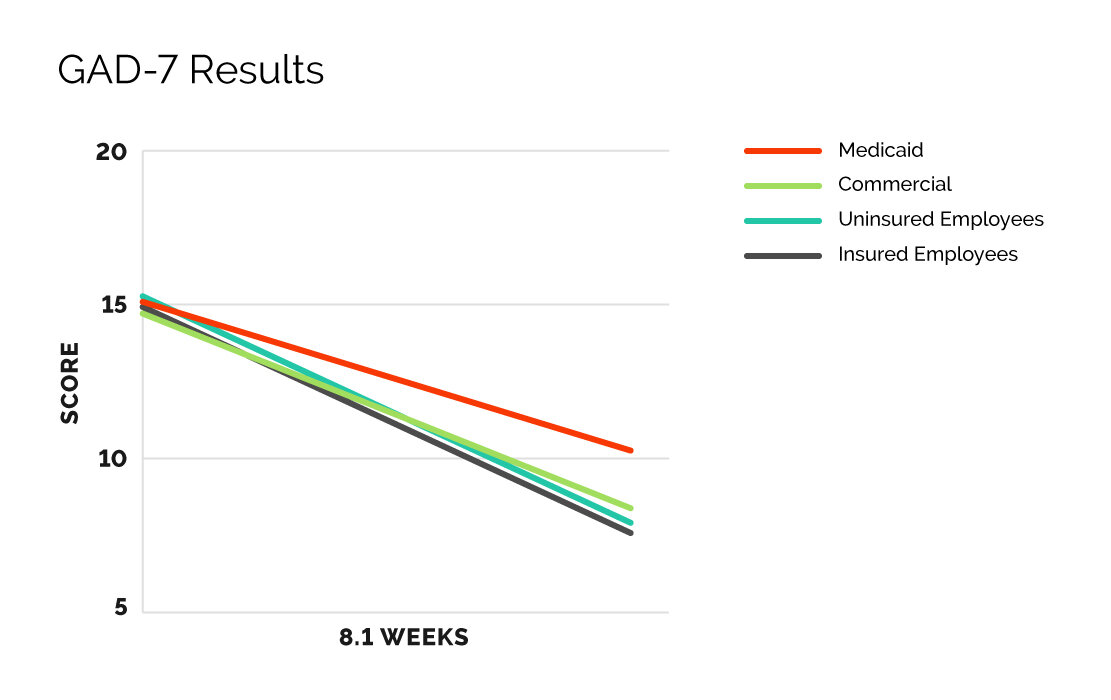
Anxiety Results by Plan Type
Unlike PHQ-9 data, there was a difference in clinically meaningful responses when the groups receiving telebehavioral health services were broken down into patient populations.
- Commercial patients averaged initial GAD-7 scores of 14.71, reducing to 8.29 or a change of 6.42 points
- Employer insured patients averaged initial GAD-7 scores of 14.99, reducing to 7.81 or a change in 7.18 points
- Employer uninsured patients average initial GAD-7 scores were 15.142, reducing to 7.982 or a change of 7.16 points
- Among Medicaid/ED High Utilizer population scores came close to clinically meaningful change. The average initial score was 15.09, reducing to 10.26 or a change in 4.83, just missing the 5 point threshold to meet the definition.
Analysis of Outcomes as it Relates to Multidisciplinary Team Approach:
CirrusMD takes an integrated approach to treating the whole patient, with a multidisciplinary team of physicians. The PCS team includes Family Medicine and Psychiatry physicians, supported by additional Emergency Medicine physicians.
Looking at analysis of both depression and anxiety again by looking at PHQ-9 and GAD-7 outcomes data, patients managed by the Multidisciplinary PCS team had clinically meaningful changes and positive outcomes in their mental health. Both are clinically significant with > 5 point changes and both were statistically significant as previously mentioned.
Conclusion
The CirrusMD approach to delivering care focuses on barrier-free care, keeping the patient at the center of care and treating them as a whole — mind and body. This study set out to analyze the first 6 months of mental health outcomes of patients who were seen and managed by our multidisciplinary Primary Care and Specialty Team Physicians.
The results presented are related to patients across various groups including Medicaid, Employer Insured, Employer Uninsured and Commercial, and are specific to patients seeking mental healthcare through psychiatric medication management.
CirrusMD physicians followed initial and final PHQ-9 and GAD-7 scores of those patients to understand outcomes related to medication management solutions.
The results of this 6 month study demonstrate that CirrusMD physicians provide virtual mental healthcare that resulted in clinically meaningful and significant changes in patients suffering with depression and anxiety. A Wilcoxon rank sum analysis demonstrates that the changes seen in initial PHQ-9 and GAD-7 scores compared to final PHQ-9 and GAD-7 scores are also highly statistically significant.
It is acknowledged that some of the patients cared for may have had access to other mental health professionals like therapists outside of our format and this study. This information was not included in this study as the focus was psychiatric outcomes based on medication management only. Future directions of similar studies could involve examination of therapy using either formal therapy solutions or self directed digital mental health tools in combination with psychiatric medication management or alone to examine the effects on patient outcomes, remission and sustainability of that remission.
References
1 - CMAJ. 2012 Feb 21; 184(3): 281–282. Enhancing the clinical utility of depression screening Kurt Kroenke, M
2 - Kroenke K, Spitzer RL, Williams JB, et al. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry 2010;32:345–59
3 - Roy-Byrne, P., Veitengruber, J.P., Bystritsky, A., Edlund, M.J., Sullivan, G., Craske, M., Shaw, S., & Rose, R., Stein, M.B. (2009). Brief intervention for anxiety in primary care patients. Journal of The American Board of Family Medicine, 22(2), 175-186
4 - Kroenke, K., Williams, J.B., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder. Archives of Internal Medicine, 166(10), 1092-1097.
5 - Valenstein, M., Adler, D.A., Berlant, J., Dixon, L.B., Dulit, R.A., Goldman, B., … Sonis, W.A. (2009). Implementing standardized assessments in clinical care: Now’s the time. Psychiatric Services, 60(10), 1372-1375.
6 - Murray CJL, Lopez AD, eds. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University Press; 1996.
7 - Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH. A 40- year perspective on the prevalence of depression: the Stirling County Study. Arch Gen Psychiatry. 2000; 57(3):209-215
8 - A System-Based Approach to Depression Management in Primary Care Using the Patient Health Questionnaire-9. RAMONA S. DEJESUS, MD; KRISTIN S. VICKERS, PHD, LPP; GABRIELLE J. MELIN, MD; AND MARK D. WILLIAMS, MD. Mayo Clin Proc. 2007;82(11):1395-1402.
9 - GAD-7 Assessment Resources developed by the VISN 4 MIRECC.
10 - Whooley MA, Simon GE. Managing depression in medical outpatients. N Engl J Med. 2000;343(26):1942-1950.
11 - Simon GE, VonKorff M, Wagner EH, Barlow W. Patterns of antidepressant use in community practice. Gen Hosp Psychiatry. 1993;15(6):339-408.
12 - Pollack MH, Endicott J, Liebowitz M, et al. Examining quality of life in patients with generalized anxiety disorder: clinical relevance and response to duloxetine treatment. J Psychiatr Res. 2008;42:1042-1049
13 - Achieving Remission in Generalized Anxiety Disorder - February 1, 2009 Laura A. Mandos, PharmD, Jennifer A. Reinhold, PharmD, BCPS, BCPP, Karl Rickels, MD Psychiatric Times, Psychiatric Times Vol 26 No 2, Volume 26, Issue2
14 - MacArthur Foundation’s Initiative. The Macarthur initiative on depression and primary care at Dartmouth and Duke: Depression management toolkit. Hanover, NH: Dartmouth; 2004.
15 - Gelenberg AJ, Freeman MP, Markowitz JC, Rosenbaum JF, Thase ME, Trivedi MH, et al. Practice guideline for the treatment of patients with major depressive disorder. 3. Washington, DC: American Psychiatric Association; 2010.
16 - Cut Points on the Patient Health Questionnaire (PHQ-9) that Predict Response to Cognitive-Behavioral Treatments for Depression Stephen M. Schueller, PhD,a Mary J. Kwasny, ScD,a Blake F. Dear, PhD,b Nickolai Titov, PhD,b and David C. Mohr, PhD. Gen Hosp Psychiatry. 2015 Sep-Oct; 37(5): 470–475.
17 - Kessler RC, Keller MB, Wittchen HU. The epidemiology of generalized anxiety disorder. Psychiatr Clin North Am. 2001;24:19-39.
18 - Rickels K, Schweizer E. The clinical course and long-term management of generalized anxiety disorder. J Clin Psychopharmacol.





