The employer healthcare benefits landscape continues to quickly evolve as several key factors drive the acceleration of change. In a recent study(1), over 100 leading benefit consultants were asked to weigh in on the changes they’re seeing in healthcare benefits, their thoughts on what priorities are most important for employers, and how their roles are changing today.
The survey reveals that shifts include an increased focus on personalized benefits and chronic condition management, as well as mental and emotional well-being. “There is more awareness of health equity issues than in the past,” noted one respondent. And while cost remains a primary focus, there is also an emphasis on outcomes and “more in-depth analysis of use vs cost vs plan utilization.” Consultants see their roles evolving beyond offering products, to focus more on pricing and utilization, population health management, and analytics.
To support the changing benefit needs of large employers and their team members, CirrusMD has increased the power of virtual physicians at the point of care. For more than a decade, CirrusMD physicians have met team members at their moment of need, beginning encounters within 60 seconds. Now with the launch of Physician-first Care & Guidance, we bring together physicians, smart technology, and integration with multiple data sources, to enable our expert doctors to guide patients through an entirely personalized care journey, leveraging the benefits and services specifically available to them.
What Do Employees Want Most?
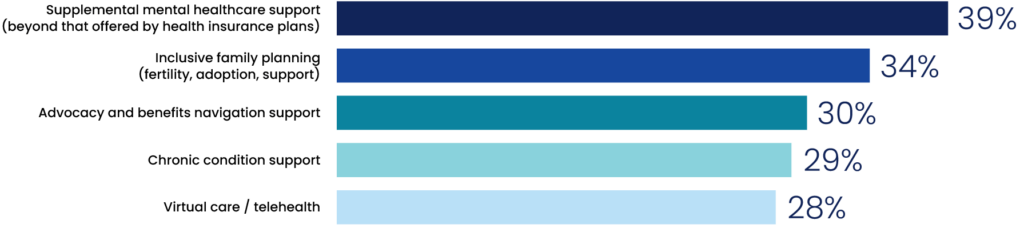
Consultants report that their self-insured employer clients say employees most often request: supplemental mental healthcare support, inclusive family planning, and advocacy and benefits navigation support. Other benefits frequently requested include chronic condition support and virtual care or telehealth options.
What Do Employers Want Most?
Cost management and health outcomes are top priorities for employers. Self-insured clients are most focused on ROI impact in the areas of cost management and health outcomes. Next in importance are member engagement and satisfaction. Operations implementation and efficiency measures made the list but with lower rankings among client priorities.
To continue to support health equity requirements, virtual care is most frequently requested by employers who recognize the opportunity for virtual solutions to cross boundaries of geography, race, culture, language, gender or other often-cited barriers to care.
What Must Navigation Provide?
When it comes to healthcare navigation, independence is cited as a key factor to the best results. More than half of consultants say they guide their self-insured clients to solutions that are unaffiliated with health plans, to tap into greater subject matter expertise, offer “more holistic and independent” service, and “generally deliver better results.” It was noted that members are often “wary of suggestions” from their insurance company, while an unbiased third party “can better evaluate all options across the landscape” and guide employees to the most appropriate provider.
CirrusMD has expanded the ability of our physicians to guide employees to their next steps in care, with a complete at scale, highly cost effective solution. Our doctors access each patient’s health information, health plan and benefits, and in-network resources, and can deliver primary, urgent/acute, chronic, and/or preventative care services immediately, as well as longitudinally, depending on what the patient needs. With a team of multidisciplinary, board-certified physicians and health coaches, CirrusMD delivers care on-demand and provides guidance and support across benefit resources and care settings, including virtual, digital, and in-person care.
According to the survey, the most important factors for self-insured employers is that their navigation solution increases cost management and control, measured in terms of per person savings, claims cost reductions and cumulative year over year savings. The second priority is health outcomes, measured through objective criteria like decreases in hospital stays, readmissions, preventive care success, chronic care quality measures. Other priorities include member engagement and utilization across services and overall employee satisfaction.
A More Integrated Model of Care & Guidance
CirrusMD’s Physician-first Care & Guidance aims to drive healthcare navigation toward a more effective model by bringing benefit navigation directly into the care encounter. Leveraging the physician as the most trusted resource, supporting them with a powerful technology platform, and giving them the time and data they need to provide personalized care, will streamline and improve the entire care experience. This new model includes more than just integration of benefits, it also includes patient health information, patient-specific benefits data, and cost & quality data. In 60 seconds or less, patients receive the evaluation, treatment and guidance they need from expert physicians throughout their care journey. With this shift, self-funded employers can drive greater benefit awareness and utilization, improve care plan adherence and health outcomes, and lower the overall cost of care for their populations.
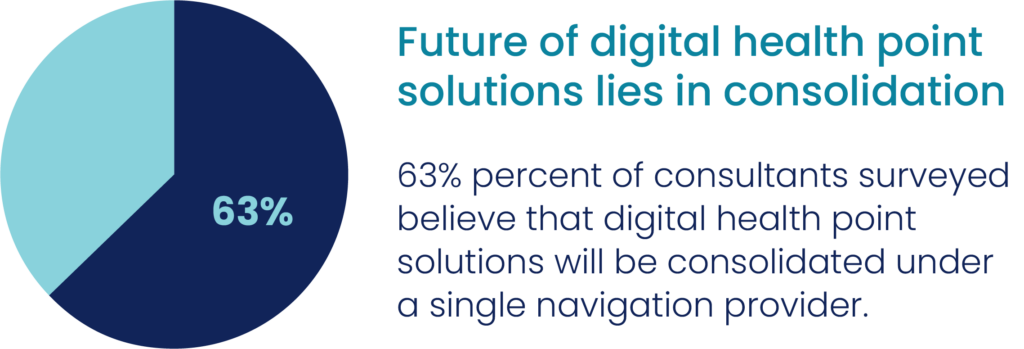
As self-funded employers look for new and innovative solutions to meet employee needs, there will undoubtedly be more shifts and consolidation of solutions and vendors. And consolidation may be helpful, if the focus is on building solutions to streamline patient journeys, deliver the most effective and cost efficient care, and reporting and data analytics to help employers truly understand the results of their benefits investments.





