The Situation: Challenges of the Care Environment
Telehealth or telemedicine has improved convenience, reduced cost, and expanded access to care for millions of Americans, but many believe the promise of care delivered virtually has not lived up to its full potential.
While patient acceptance of virtual care has grown, challenges have remained. First-generation telehealth solutions simply replicate an in-person office visit with a video visit over the web. While this improved access for patients whose concerns could be treated remotely, it’s done little to improve efficiency for the physician, and in many cases, has created additional stress and burn-out as doctors try to balance the demands of their in-person and remote patients(1). Additionally, gen-1 solutions tend to be transactional in nature, fee for service based, and disconnected from other settings that may be an essential part of a patient's health journey. As a result, plan sponsors must weigh concerns about the quality and continuity of their virtual care programs.
In fact, for every stakeholder in the healthcare ecosystem virtual care has been a mixed blessing:
- For physicians, access to telehealth solutions has allowed them to reach more patients, but without efficiency gains and or the benefit of information that would help manage a more dynamic patient load. The result has been a more transactional experience for patients and heightened levels of stress and burn out for doctors.
- For patients, while there is value in care delivered remotely, cost effectively, and in many instances far more quickly, gen-1 solutions still have numerous restrictions, including limitations in the kinds of care delivered virtually; the transactional nature of care delivered; the lack of a holistic patient view; and the missing integration with other care settings. Additionally, virtual care solutions have required patients to have equipment, privacy, and bandwidth to participate in each encounter.
- For plan sponsors, employers and health plans who pay for much of a patient’s healthcare costs, the savings associated with care redirected from ER and urgent care settings must be balanced with the quality of care delivered and continuity of care for members dealing with long-term, complex, and chronic conditions.
For all of the benefits that virtual care has delivered to physicians, patients, and plan sponsors, there is still much to be done to unleash the full value and promise of virtual care to improve care delivery in the U.S.

What’s Missing from Today’s Virtual Care Solutions
What’s needed to realize the full potential of virtual care is a complete reimagining of how to apply its unique attributes with human-centered design to create a new, purpose-built care delivery model that is fully integrated into all elements of the healthcare ecosystem. One that supports the expansion of Primary Care for all by providing consistently high-quality, empathetic, and accessible care for patients; efficiency and sustainability for providers; and consistent savings for plan sponsors.
We have the tools and, post-COVID, we now have the experience with virtual care to implement a new generation of solutions that leverage capabilities like asynchronous communication, new AI tools, data warehouses, remote monitoring devices, and patient-controlled information to finally deliver a “virtual point of care” that works for all stakeholders. That’s how we create a better encounter, a better point of care, and ultimately better primary care for our members.
— Jamie Hall, President & CEO, CirrusMD
The Industry Perspective
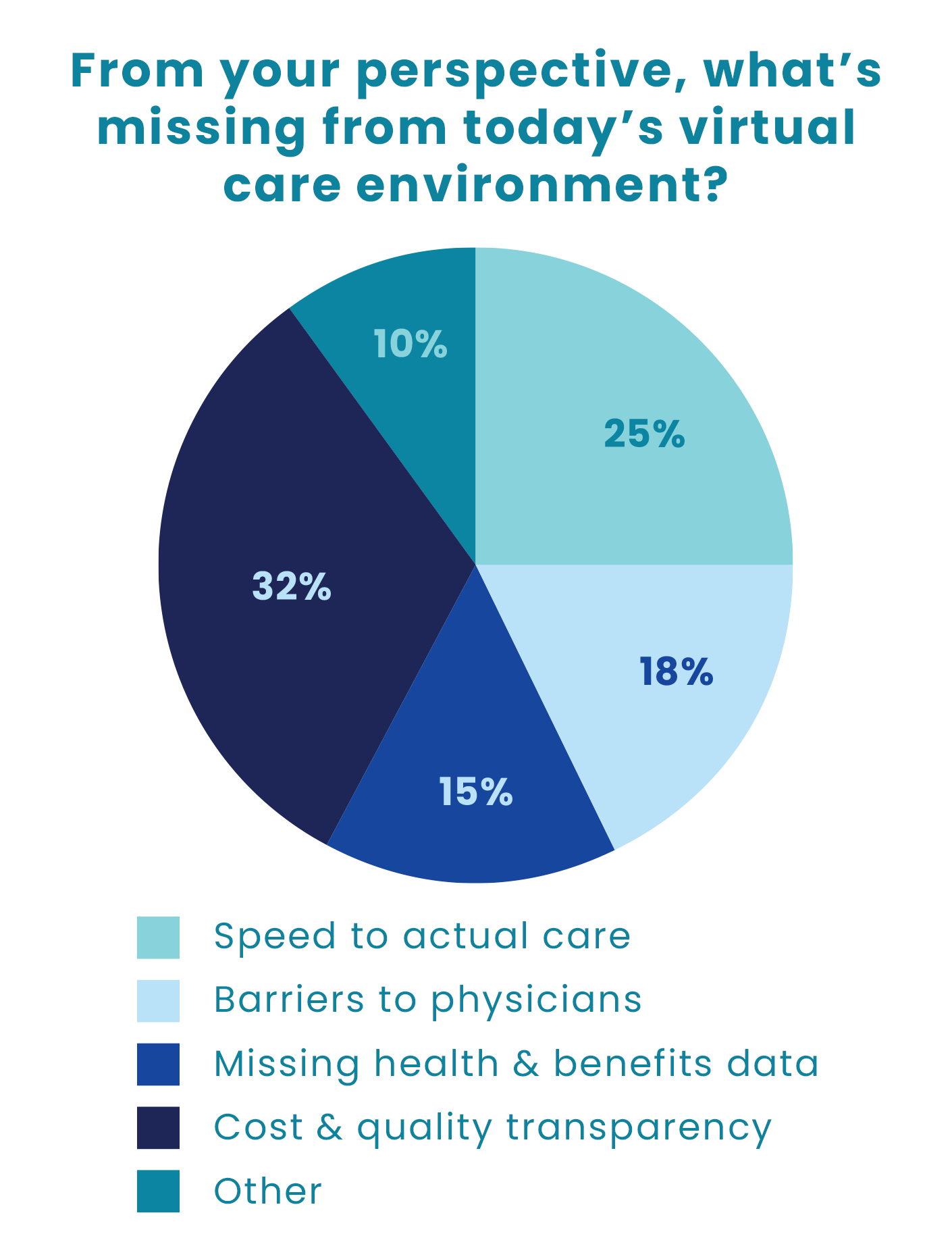
CirrusMD researchers posed a single question to a broad audience made up of health plans, employers, brokers & consultants, and other industry thought leaders:
“From your perspective, what’s missing from today’s virtual care environment?”
This report provides a more comprehensive analysis of the four primary issues restricting the full value of virtual care solutions today. Addressing these issues is not only critical for enhancing the effectiveness of virtual care, but also to unlocking greater value to all healthcare stakeholders.
Examining the Issues

Speed to Care: Enhancing Efficiency and Satisfaction
Quick and frictionless access to care is essential to both the efficiency and effectiveness of healthcare delivery. From diagnosis and treatment to follow-up and referrals, closing the gap in speed to care delivers compelling benefits.
- Facilitating quick and easy access to physician-first care supports early diagnosis and treatment, which improves health outcomes. By promptly connecting patients with doctors, we can identify and address health concerns in their nascent stages, preventing the progression of illnesses to improve and even save lives.
- Accelerating care delivery enables individual benefits as well as a broader societal impact. Virtual care is easier to access and can alleviate the burden on brick and mortar resources while reducing healthcare costs. By diverting patients away from costly and resource-intensive care settings, we can optimize resource allocation and improve the efficiency and effectiveness of the healthcare system.
- In an era of on-demand services, patients increasingly value quick and convenient access to care. Speed to care not only enhances medical outcomes but also elevates the patient experience. By meeting the member in their moment of need, the moment when they determine care is needed, we increase satisfaction and trust, enabling a more patient-centric healthcare ecosystem, where individuals feel heard, valued, and promptly attended to.
To improve care delivery, speed is not merely about convenience; it is a vital factor in both the quality and competency of our healthcare. By reducing the time it takes to connect with a doctor, we support early intervention, reduce healthcare burdens, and heighten patient satisfaction to shape a more efficient and effective care model for all.

Barriers Between Patients and Physicians: Closing the Gap to Improve Care
Speed to a doctor is essential to the quality and effectiveness of our healthcare; however, the growing scarcity of physicians in the U.S. has increased the distance between patient and provider. To alleviate the burden on physicians, a new generation of digital tools (apps, bots, and portals) and non-clinical navigators have been developed to provide patient support without the need for a doctor visit. While many of these resources have improved access to resources and information, they cannot replace the impact of a physician’s educated care and guidance throughout a patient’s healthcare journey.
The Provider Shortage in the U.S. and Its Impact on Care Delivery
Today the U.S. has fewer general physicians per capita than our parity nations, which include Australia, Austria, Japan and Germany. In the U.S. only 12% of physicians are generalists (vs. 44% in Australia), there are fewer physicians per capita (2.6 per thousand vs. 5.2 per thousand in Austria), and fewer psychologists and psychiatrists working in mental health than most comparable countries(2).
Provider scarcity will be a growing problem as multiple surveys indicate that a “great clinician resignation” lies ahead. According to a March 2022 AMA survey of 9000 physicians, 1 in 5 plan to exit their practice in the next 2 years. These results are more acute in the primary care setting. Another 2022 survey estimated 25% of clinicians planned to leave primary care within 3 years.
Primary Care Physician (PCP) dissatisfaction is attributed to burnout, stress, COVID fatigue, increasing administrative/documentation burden, poorly populated electronic health records, shortages of support staff, and increased patient volumes.
How does the physician shortage affect patients and ongoing care?
With the following adjustments in how we deliver care, we can simultaneously alleviate the burden on physicians and improve access.
- The physician is the most trusted resource in healthcare(3). Placing the physician at the beginning of every healthcare journey is pivotal to implementing a new, more effective model of care. By realigning digital and navigation tools in support of the patient-physician relationship, we can deliver a more seamless, efficient, and patient-centric care experience.
- Chat-enabled virtual care makes scalable, physician-first care possible. It paves the way for new staffing and care delivery models, expanded encounter windows, real-time peer-to-peer support, and asynchronous exchange between patients and physicians. As a result physician-first care is both possible and scalable, relieving the burden on physicians, strengthening peer relationships, reducing stress, and even improving physician satisfaction – all while creating greater access for patients.
- Data supports better decision-making; however, physicians need to distinguish the critical signals quickly and easily from the noise arising within patient data. Leveraging artificial intelligence to surface the right information to doctors at the point of care streamlines the healthcare experience and sets both patient and provider up for greater success. This reduces the burden for both patient and physician – further improving care delivery and driving greater satisfaction for all parties.
By realigning today’s technology and healthcare resources to support the physician and the physician-patient relationship, the burden on providers is greatly reduced and physicians are optimized to deliver better care. This further enhances the virtual care experience for patients and physicians.

Missing Health and Benefits Data: Delivering Vital Information to Physicians
One of the most significant barriers to effective care (whether virtual or brick and mortar) comes from the lack of physician access to patient health information, including current health status, chronic conditions, health risks, and importantly, care benefits available through their plan sponsor. Bringing together the trusted physician with the most relevant and contextual information about the patient supports a better care journey from start to finish. With this information in hand, physicians can create a more informed treatment plan and guide patients through the completion of their care journey.
- Smart technology platforms can ingest patient data from multiple sources, including structured and unstructured encounter data; self-reported patient data; claims; HIE (Health Information Exchange) and cost and quality data; and, plan sponsor data such as benefit resources, point solutions, and SPDs (Summary Plan Descriptions) to support the doctor in choosing the best resource based on the patient’s specific care needs.
- Trained physicians at the forefront of the care experience are the best and most trusted clinical resource to use such information to diagnose and treat patients specific to the patient’s needs, health risks, and medical history. This enhances the quality of care, contributes to more effective, targeted medical interventions, and improves treatment adherence rates – addressing both immediate health concerns and long-term wellness objectives.
- Generative AI can make it easier for doctors to create personalized treatment plans for patients to follow. Technology today can identify underlying health risks and patient concerns during the care encounter. It can surface the patient’s relevant health information and any corresponding plan-sponsored resources at the same time. This means physicians receive actionable data points to share with the patient when the patient is most engaged.
Data drives better-informed decisions. Addressing incomplete patient information is not simply a convenience but a critical step toward elevating the quality of the patient care experience, setting the patient on a path toward better health from the first step.

Lack of Transparency to Cost and Quality: Physician Guidance to Next Best Step
As the healthcare ecosystem increases in complexity and fragmentation, stakeholders feel the fall-out. The lack of transparent cost and quality data was ranked by survey respondents as the most significant gap in virtual care solutions. It’s reported that patients face challenges in understanding healthcare options, navigating insurance coverage and benefits, and accessing appropriate care, in turn leading to suboptimal health outcomes and increased costs.(4)
- While virtual care can support a significant percentage of a patient’s care needs, there are times when an in-person care setting is most appropriate. A physician-directed virtual care model means physicians leverage cost and quality data to guide patients to the next best step in their care journey – including clinical services and care delivered in brick and mortar settings. When referrals are made without guidance or cost and quality insights, it can create a more fragmented experience.
- This issue extends beyond mere convenience. Fragmented care can negatively impact the quality and costs of care delivered and ultimately, the patient experience. While healthcare navigation platforms are emerging as a solution to address the challenges of complexity and lack of transparency,(6) physicians with the right information at hand can better support patient guidance to the most appropriate, affordable, high-quality care – further streamlining the care journey.
- Greater transparency of cost and quality metrics assume a crucial role in enabling patients to assess the competence and reliability of their care providers, yet not all patients feel qualified to understand these metrics. In a physician-directed virtual care model, cost and quality information can support patients with important information needed for their healthcare journey, clarifying available resources and associated costs. In this model, referrals from trusted physicians are well aligned with the patient’s needs, improving treatment plan adherence and further reducing fragmentation.
OF AMERICANS REPORTED THEY OR FAMILY MEMBERS POSTPONED TREATMENT DUE TO COSTS
%
INCREASE FROM 2021 TO 2022
%

As these barriers are removed from the care system, we will begin to measure improved patient outcomes, reduced healthcare costs, increased patient engagement, enhanced healthcare equity, and a more consumer-centric healthcare system. A physician-first model of virtual care becomes a pillar of the overarching care ecosystem, delivering efficient, accessible, and patient-centered services.
This emerging model of physician-first care and guidance will not only benefit individual patients but also contribute to a more effective and sustainable healthcare ecosystem in the future.